The UK faces an astonishing challenge: misdiagnosis in heart failure ranges from 16% to 69% depending on setting. This scale reveals why better tools are urgent across the NHS.
Modern cardiology now gathers vast signals and images from ECG, ultrasound, CT and X‑ray. Artificial intelligence can automate measurements and standardise interpretation to cut uncertainty and variation.
Early adopters report major gains: pre‑populated echo reports up to 83%, hybrid theatres doubling structural case volumes and turnover time reductions of 50–75%. These are signs that technology can speed workflows and protect patients through dose‑optimised imaging.
This section outlines how rich clinical data become actionable insight, and why adoption matters for care, outcomes and the future of heart services. For an evidence summary on predictive analytics and clinical impact see recent research.
Key Takeaways
- Misdiagnosis is common: rates vary widely and drive the need for better tools.
- Automated measurements improve consistency and speed in routine reporting.
- Multimodality imaging fusion links anatomy to function for more accurate decisions.
- Operational gains include faster workflows and safer, dose‑optimised imaging.
- Adoption in the NHS must balance productivity with governance and workforce training.
Why AI in cardiology matters now in the UK health system
Pressures on UK heart services mean teams must turn vast clinical records into clear, timely decisions.
From data-rich specialties to actionable intelligence
The UK’s cardiology departments collect large volumes of imaging and signal data from ECG, ultrasound, CT and X‑ray.
Automated measurement and standardised interpretation make that information easier to trust. Systems that pre-populate echo reports can cut reporting time and improve reproducibility.
Bridging resource limits to speed diagnosis and treatment
Clinicians face staffing and capacity constraints that delay care. Misdiagnosis of heart failure has been reported between 16% and 69%, underlining the need for earlier risk detection.
Real-time prioritisation tools help teams reduce bottlenecks and compress time-to-diagnosis, so patients receive the right treatment sooner.
“Practical tools that support judgement, rather than replace it, deliver the fastest gains for patients and teams.”
| Challenge | Practical gain | Impact on patients |
|---|---|---|
| High imaging volume | Automated measurements | Faster, consistent diagnosis |
| Staff shortages | Workflow prioritisation | Reduced delays to treatment |
| Variable interpretation | Standardised reports | Better outcomes and less risk |
- Deployment should be clinician-led and align with UK guidelines.
- Focus on near-term, measurable gains in cardiovascular medicine and medicine practice.
Imaging revolution: AI-enhanced echo, CT, MRI and X‑ray for sharper diagnosis
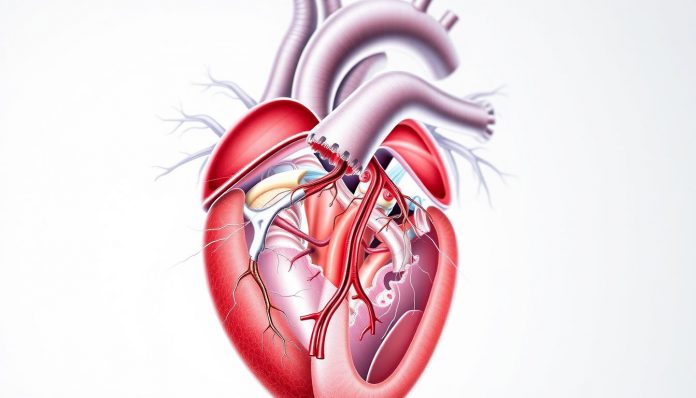
Modern imaging systems combine faster acquisition with smarter processing to sharpen clinical decisions. These technologies standardise outputs and reduce repeat scans, so teams spend less time chasing measurements and more time treating patients.
Automated measurements and segmentation to reduce variability and errors
Machine-learning tools in echocardiography now match experienced operators at segmenting chambers and producing consistent measurements across common views. This reduces inter- and intra-operator variation and cuts reporting time in busy departments.
Fusing multimodality data to see coronary stenosis and downstream functional effects
Combining 3D CT angiography that shows coronary artery stenosis with cardiac MRI or molecular scans clarifies both anatomy and perfusion. Such fusion of imaging and clinical data gives clinicians a fuller picture for suspected coronary disease—an example of better diagnosis and planning.
Radiation dose optimisation and safety while maintaining image quality
Guided imaging technologies and algorithms monitor dose in real time, preserving image quality while enhancing safety for patients and cath lab staff. Deployments in hybrid theatres have increased throughput and improved turnover without compromising quality.
- Standardised segmentation and automated measurements cut errors and speed reporting.
- Multimodality fusion links stenosis to function for clearer therapeutic choices.
- Dose‑optimised protocols safeguard staff and patients while keeping diagnostic value.
ECG and arrhythmia: deep learning adds a new layer of interpretation
Wearable and ambulatory traces are uncovering silent electrical markers that predict future heart failure.
Deep learning now matches or outperforms cardiologists for many rhythm classifications on ambulatory ECGs.
These models scale reliable rhythm recognition across large caseloads and reduce missed events.
From rhythm recognition to pre-symptom screening
Trials show that an automated ECG screen can flag asymptomatic patients at higher likelihood of reduced ejection fraction.
A positive result associates with roughly a fourfold greater future risk of low EF, prompting timely imaging and guideline-based therapy.
- Deep learning enhances ECG interpretation beyond human pattern recognition for routine use.
- Algorithms can detect likely low EF before echo changes are visible, enabling earlier intervention.
- For arrhythmia care, tools help cardiologists prioritise significant events and keep auditable records.
- Longitudinal modelling of disease pathways such as atrial fibrillation may guide treatment selection and monitoring intensity.
“ECG screening offers a low-cost, non-invasive layer that precedes imaging evidence and focuses resources on higher‑risk patients.”
| Feature | Practical benefit | Clinical action |
|---|---|---|
| Automated rhythm classification | Faster triage of traces | Prioritise urgent review |
| EF risk prediction from ECG | Early detection of latent dysfunction | Schedule confirmatory echocardiography |
| Longitudinal modelling | Risk stratification over time | Inform ablation or anticoagulation decisions |
Robust validation and clinician oversight remain essential so that ECG systems augment diagnosis and avoid over‑calling benign findings.
From diagnosis to therapy: precision cardiology and patient-specific pathways
Precision therapy is moving from broad guidance to care plans tailored for each patient’s heart.
Predictive tools use machine learning to forecast disease progression and guide therapy selection. For example, models can predict response to cardiac resynchronisation therapy (CRT) before implantation. This may avoid non-response in roughly one-third of patients and focus resources on those most likely to benefit.

Predicting progression and choosing treatment
Collaborations now model atrial fibrillation trajectories to inform rhythm versus rate strategies and procedural timing.
Using diverse data to individualise care
Integrating imaging, biomarkers, device logs and home monitoring powers algorithms that anticipate complications and tailor follow-up. Post-discharge signals can predict recovery and reduce readmissions by adapting medication and clinic reviews.
“Patient-centred pathways should match predicted risk to care intensity, not the other way round.”
- Personalised models move beyond averages and shape shared decisions.
- Predictive CRT tools reduce unnecessary implants and improve overall outcomes.
- Heterogeneous data streams let clinicians individualise treatment and monitor results in near real time.
Clinician workflows reimagined: productivity, reporting and hybrid theatres
Operational intelligence is changing the pace of cardiology care and what a typical shift looks like.
Pre-populated echocardiography reports now cover up to 83% of routine fields. This reduces manual entry and boosts reproducibility of measurements.
Faster reporting and reproducible measurements
Machine-assisted reporting and standardised outputs speed discharge and free clinicians for direct patient care.
Such tools cut variation and shrink time spent on documentation.
Digitally driven theatres and cath labs
Hybrid operating rooms can scale throughput: Aurora St. Luke’s doubled daily structural cases from 3 to 6 and cut turnover by 50–75%.
Integrated technologies combine imaging, haemodynamics and guidance in one environment without loss of quality.
Real-time logistics and safer practice
Department dashboards detect bottlenecks and issue alerts so teams prioritise patients and reallocate staff swiftly.
Guided imaging and dose optimisation protect operator and patient safety during long X‑ray cases.
- Tools that pre-fill notes reduce admin time and variation.
- Machine scheduling trims delays and improves list efficiency.
- Secure email alerts coordinate multidisciplinary responses and speed discharge planning.
| Feature | Practical gain | Clinical effect |
|---|---|---|
| Pre-populated reports | Up to 83% automation | Faster, consistent reporting |
| Hybrid theatre integration | Double case volumes; 50–75% turnover reduction | Increased capacity and revenue |
| Real-time dashboards | Immediate bottleneck alerts | Priority scheduling and fewer delays |
| Dose optimisation | Monitored radiation | Improved staff and patient safety |
Prevention at scale: opportunistic screening and earlier cardiovascular disease detection
Hidden cardiovascular risk often sits unnoticed in archives of chest CTs and ambulatory ECGs. Opportunistic screening mines that routine clinical data so whole groups of people can be assessed without extra visits.

Mining existing scans and ECGs to surface hidden risk in broader populations
Incidental coronary artery calcium on chest CTs stratifies cvd risk. Agatston scores above 100, from deep learning models, mark substantial hazard and can prompt statin discussions.
In one Bay Area cohort without known atherosclerotic disease, 50% had some coronary calcium. EchoNext found 9% of patients with an ECG were high risk for structural disease, yet 45% lacked follow-up echocardiography.
Clinical trials and live inferences: building screening pipelines in practice
Large pipelines copy new studies, run models and generate live inferences. Columbia’s system has processed one million patients and completed five clinical trials, showing how screening can run in the background.
“Embedding screening into routine workflows reaches patients who do not attend preventive clinics.”
- Screening can be automatic and population‑wide.
- Automated pathways expose gaps: many high‑risk patients need recall by phone or email.
- AI‑guided amyloidosis screening found 48% positives and 91% of those started treatment, an example of direct benefit.
How Will AI Transform Cardiology? Find Out Now!
Digital literacy and inclusive design determine whether new tools narrow or widen health gaps.
Equity and sex-sensitive models
Algorithms can reduce gender bias by using sex-aware thresholds and sex-specific features such as troponin trends. Models trained on diverse population samples help ensure fair performance for women and men across age groups.
Equitable design must include validation for cardiovascular disease and cvd presentations common in women. That prevents missed diagnoses and improves follow-up rates.
Governance, accountability and clinician leadership
Clear frameworks should state who is accountable when algorithms err and how outputs inform clinical decisions. Cardiologists must lead validation, set standards and guide public communication.
“With many patients already using generative tools, clinician oversight protects trust.”
Workforce training and digital inclusion
Medical education should add algorithmic learning and basic computer science so future clinicians can appraise models. Continuous professional learning will keep practice safe as technology evolves.
- Build algorithms from representative data and focus on women’s presentations.
- Define responsibilities for errors and integrate outputs into pathways.
- Support patients with clear materials, community training and secure email contact.
- Shape measured regulation led by clinical teams over the next decade.
Conclusion: How Will AI Transform Cardiology? Find Out Now!
Embedding validated models into routine practice offers a clear route to better care. Across imaging and ECG, automated measurements, dose‑optimised procedures and screening pipelines already reveal hidden risk and prompt timely treatment for many patients.
Evidence from trial platforms and large programmes shows tangible gains in workflow, capacity and outcomes when practical tools and clinician oversight work together. Hybrid theatres and accelerated reporting are examples that improve throughput and patient pathways.
Success depends on governance, diverse training data and workforce education so cardiovascular medicine benefits equitably. With clinician leadership and measured evaluation, this way of working can improve outcomes and make the best use of data generated across UK services.
For more Healthcare and Technology articles, please follow the link