What if the key to tackling one of our most devastating neurological conditions lies not in the brain’s neurons, but in its protective shield? A remarkable international study is forcing scientists to reconsider the fundamentals of Alzheimer’s disease.
Researchers have achieved a stunning reversal of symptoms in animal models. This was accomplished using innovative bioactive nanoparticles. The approach represents a significant shift from traditional methods.
Alzheimer’s disease progressively destroys memory and cognitive skills. It affects millions globally. The condition is characterised by a harmful build-up of proteins, like amyloid plaques, which disrupt normal brain function.
This novel treatment targets the blood-brain barrier itself. By repairing this vital gateway, the therapy allowed the brain to begin healing. The success in mice offers a hopeful new direction for disease research.
Key Takeaways
- An international team of scientists has successfully reversed Alzheimer’s symptoms in laboratory mice.
- The new therapy utilises bioactive nanoparticles to target the root causes of the disease.
- Alzheimer’s disease is characterised by the accumulation of harmful proteins, such as amyloid plaques, in the brain.
- This approach focuses on repairing the blood-brain barrier, a novel strategy compared to previous treatments.
- While a promising breakthrough, this research is in its early stages and requires further investigation.
- The findings open up a potentially transformative new pathway for treating dementia and related conditions.
Emerging Insights in Alzheimer’s Research
Modern Alzheimer’s investigations are challenging long-held assumptions by exploring how blood-brain barrier dysfunction contributes to cognitive decline. This represents a significant departure from earlier research that primarily targeted neurons and brain cells.
Recent Breakthroughs and Novel Approaches
The historical evolution of Alzheimer’s studies shows a clear progression. Early therapeutic attempts concentrated on neural pathways. Contemporary approaches now investigate multiple contributing factors.
Vascular health and protein clearance mechanisms have emerged as critical areas. This paradigm shift reflects growing evidence that successful treatment requires a multi-system approach.
Innovative Nanotechnology and Clinical Trial Updates
Researchers have developed a revolutionary technique using nanoparticles as bioactive agents. Unlike traditional nanomedicine that uses particles as delivery vehicles, this study employs “supramolecular drugs” that act directly on biological targets.
The approach targets the LRP1 protein specifically at the blood-brain barrier. This structure serves a dual purpose: protecting the brain from toxins while facilitating drug delivery.
According to recent findings, restoring barrier function represents a promising new avenue. Experts emphasise that vascular repair could transform how clinicians approach this disease.
Leading scientists from institutions like Imperial College London note the barrier’s protective nature also hampers waste removal. This accumulation contributes significantly to Alzheimer’s disease progression.
The broader context of clinical trials suggests multiple therapeutic strategies will be necessary. These findings contribute to accumulating evidence for enhanced clearance mechanisms.
Mice Cured of Alzheimer’s with Breakthrough Treatment
Groundbreaking research indicates that targeting vascular structures can lead to significant improvements in neurological function. The experimental approach demonstrates significant potential for addressing neurodegenerative conditions.
Reversal of Amyloid Plaques and Tau Tangles
The treatment achieved remarkable results in reducing harmful protein accumulation. Researchers observed a 45 percent decrease in overall amyloid levels.
Within just one hour after injection, amyloid-beta amounts inside the brain dropped by 50-60 percent. This rapid clearance indicates the effectiveness of the nanoparticle approach.

Junyang Chen from West China Hospital noted the striking speed of this clearance. The bioactive particles facilitate the removal of toxic species that disrupt normal brain function.
Cognitive Restoration and Synaptic Connectivity
Behavioral tests revealed significant improvements in spatial learning and memory capabilities. Treated animals performed at levels comparable to healthy counterparts.
A compelling case involved a 12-month-old mouse equivalent to a 60-year-old human. After receiving three doses and observing for six months, the 18-month-old animal showed complete recovery.
Lorena Ruiz Perez highlighted the restoration of healthy barrier function. This led to a striking reversal of Alzheimer’s pathology and sustained benefits for up to six months.
Synaptic connectivity improved as toxic proteins were cleared. Neuronal communication regained effectiveness, supporting proper memory formation and cognitive processing.
Discover how healthcare is balancing the power of AI with crucial ethical principles.
Advances in Treatment Mechanisms and Future Perspectives
The molecular engineering behind this therapeutic strategy represents a fundamental shift in how scientists approach neurodegenerative conditions. Unlike traditional methods, these supramolecular drugs mimic the natural ligands of the LRP1 protein, which usually clear amyloid-beta from the brain.
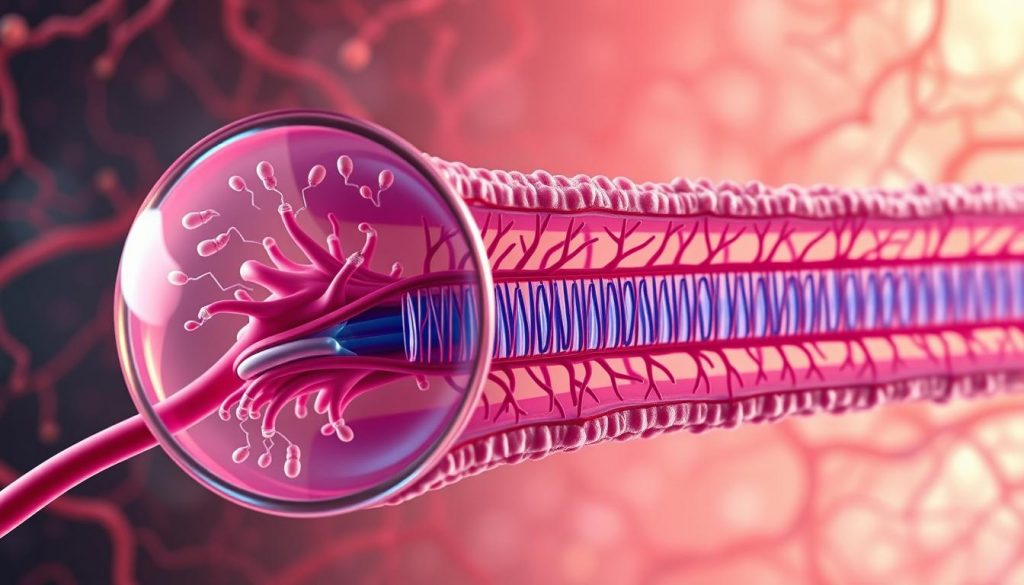
Professor Giuseppe Battaglia from the Institute for Bioengineering of Catalonia explains the cascade effect. “Once vascular function is restored, it begins clearing harmful molecules. This allows the entire system to recover its natural balance.”
Monoclonal Antibody and Gene Therapy Strategies
Future treatments may combine this approach with monoclonal antibodies. These targeted drugs could work alongside nanoparticle therapy for enhanced effect. Gene therapy strategies also show promise for addressing underlying causes at the cellular level.
Significance of the Mouse-to-Human Gap and Safety Considerations
Human blood-brain barriers are far more complex than those in laboratory models. This difference explains why many promising studies fail in human trials. Professor Tara Spires-Jones cautions that these findings need extensive replication.
Considerable research remains to be conducted before determining safety in human patients. The study published in Signal Transduction and Targeted Therapy represents early experimental work. Researchers must address species differences in vascular function before applying their findings to clinical settings.
Conclusion
By focusing on the brain‘s vascular health, scientists are opening a new frontier in the fight against dementia. This research demonstrates that repairing the blood-brain barrier with bioactive nanoparticles can reverse pathological processes, facilitating the clearance of toxic proteins and restoring cognitive function for several months.
The findings, detailed in a recent report, highlight a significant shift from targeting neurons to supporting the brain‘s natural defense systems. This approach underscores the critical role of vascular function in Alzheimer’s disease progression and decline.
While this study represents a hopeful advance, the path to human treatment remains a complex one. Given that over a million people in the UK live with dementia, this type of innovative research is urgently needed. It brings science a vital step closer to future therapies that could meaningfully alter the course of the disease.


